Table of Contents
Perhaps you or your family are at a loss due to the diagnosis of multiple myeloma (MM). Understanding the disease is the first step in managing it, and having a correct understanding of multiple myeloma helps to eliminate panic and encourage active treatment. So, what exactly is multiple myeloma?

What is Multiple Myeloma?
Multiple myeloma is the second most common hematologic malignancy1, occurring in bones and other parts of the body. In patients with myeloma, the myeloma cells in the bone marrow become so numerous that they crowd out healthy blood cells, leading to clinical symptoms such as blood problems2.
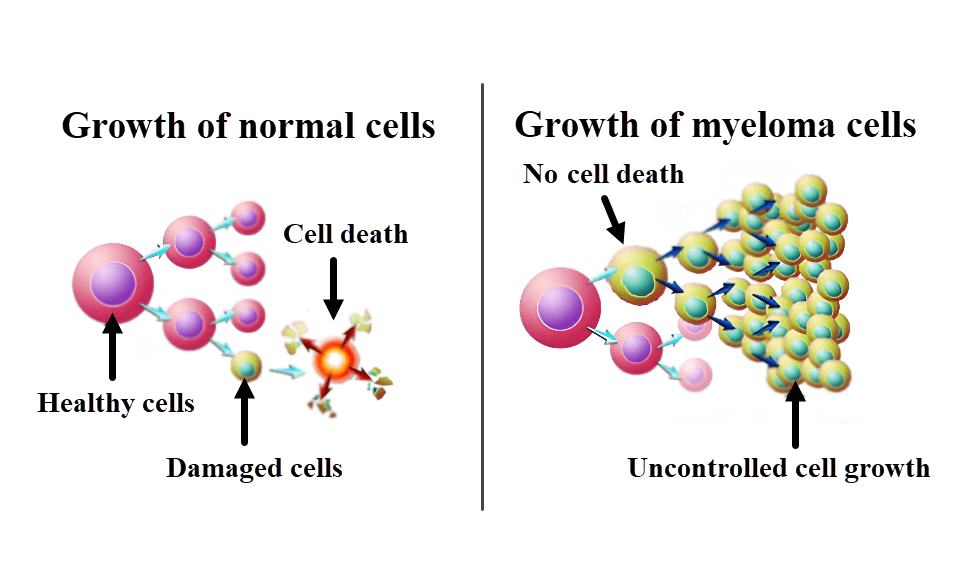
How Does Multiple Myeloma Develop?
The exact cause of multiple myeloma is not yet clear, but it is currently thought to be related to exposure to radiation or contact with chemical solvents. Toxic chemicals that have been proven to be associated with the development of multiple myeloma include cleaning agents, pesticides, fuels, solvents, engine exhaust, benzene, and dioxins3.
The Occurrence And Development Of Multiple Myeloma
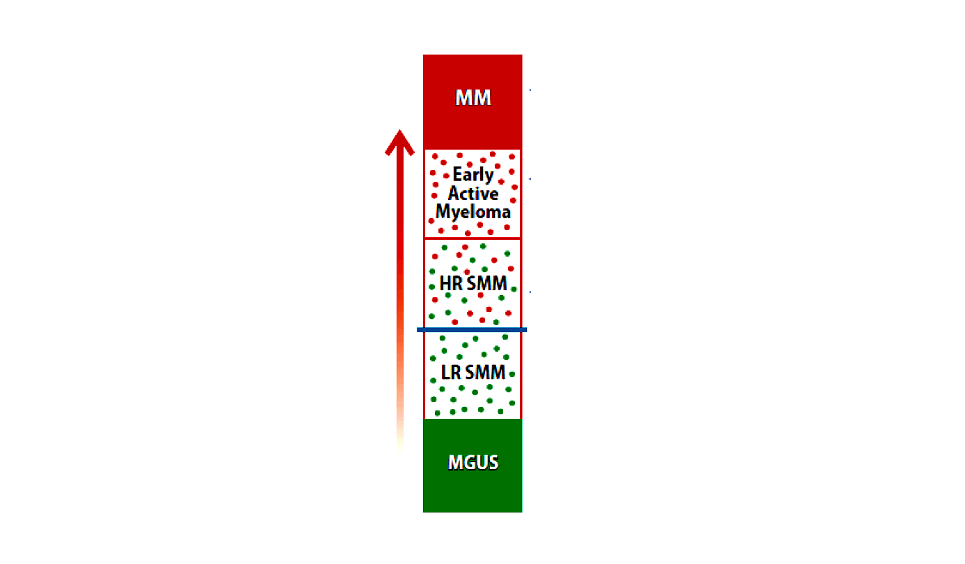
The pathogenesis of multiple myeloma is a complex process of malignant clonal replication of plasma cells, which is not yet fully understood. It usually develops from asymptomatic monoclonal gammopathy of undetermined significance (MGUS) and smoldering multiple myeloma (SMM).
MGUS is a precancerous lesion, some of which can develop into multiple myeloma, with MGUS progressing to myeloma at a rate of about 1% per year. MGUS gradually develops into SMM, also known as asymptomatic MM4, with standard-risk SMM progressing to active myeloma at a probability of 10% within the first five years5. Patients with high-risk SMM may require more frequent follow-ups or even treatment. But for most people, it takes many years for SMM to progress to multiple myeloma2.
Clinical Symptoms Of Multiple Myeloma
Common clinical symptoms of multiple myeloma include bone pain (usually in the back), fatigue, and frequent infections. The appearance of clinical symptoms is due to myeloma cells and M proteins reducing the number of normal blood cells and antibodies, disrupting the function of blood, organs, and other parts of the body.
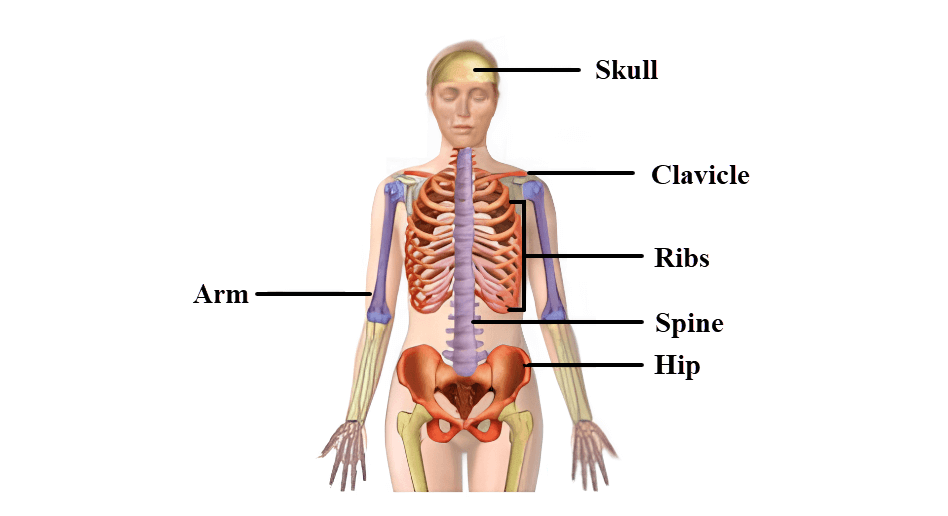
Bone injury and pain
When myeloma cells crowd out normal cells in the bone marrow, it leads to bone injury. Myeloma cells also release chemicals that break down bones. The areas of bone injury are called lytic lesions, which can lead to severe pain. Bone lesions also weaken the bones, making patients prone to fractures2.
Fatigue and asthenia
Fatigue refers to feeling severely tired despite adequate sleep and rest. Fatigue, asthenia, and “brain fog” (unclear thinking) may be symptoms of anaemia. One of the causes of anaemia may be the large number of myeloma cells crowding out the red blood cells in the bone marrow2.
Thirst and pollakiuria
High levels of M protein produced by myeloma cells can lead to kidney injury. When bone damage occurs, calcium is released into the bloodstream. High levels of calcium in the blood (hypercalcaemia) also cause kidney injury. Worsening kidney function can further increase calcium levels, creating a vicious cycle.
An increase or decrease in urine output may be a symptom of kidney injury. It may also lead to extreme thirst, confusion, nausea, constipation, muscle twitching, bone pain, or other related symptoms2.
Vulnerable to bruise or bleeding
Platelets are blood cells that help with wound healing and haemostasis, but an excess of myeloma cells can crowd out the haematopoietic stem cells and normal haematopoietic cells in the bone marrow (including megakaryocytes that produce platelets), leading to a reduction in platelets
Symptoms of thrombocytopenia (platelets decreased) include easy bruising or bleeding, such as nosebleeds and bleeding gums2.
Frequent infection and pyrexia
Fever is a sign that the body is trying to fight off an infection, and myeloma cells replacing normal plasma cells lead to a reduction in antibody production.
Frequent fevers and infections are symptoms of low normal antibody levels and a shortage of white blood cells (infection-fighting cells). An excess of myeloma cells in the bone marrow may lead to a reduction in white blood cells2.
How Is Multiple Myeloma Diagnosed?
If your doctor suspects you have myeloma, several medical investigations are required before treatment can begin. Some investigations are used to check your general conditions. Other investigations are for diagnosing the disease. All these investigations help the doctor determine if you need treatment and which treatment is best suited for you2.
Risk Stratification Of Multiple Myeloma
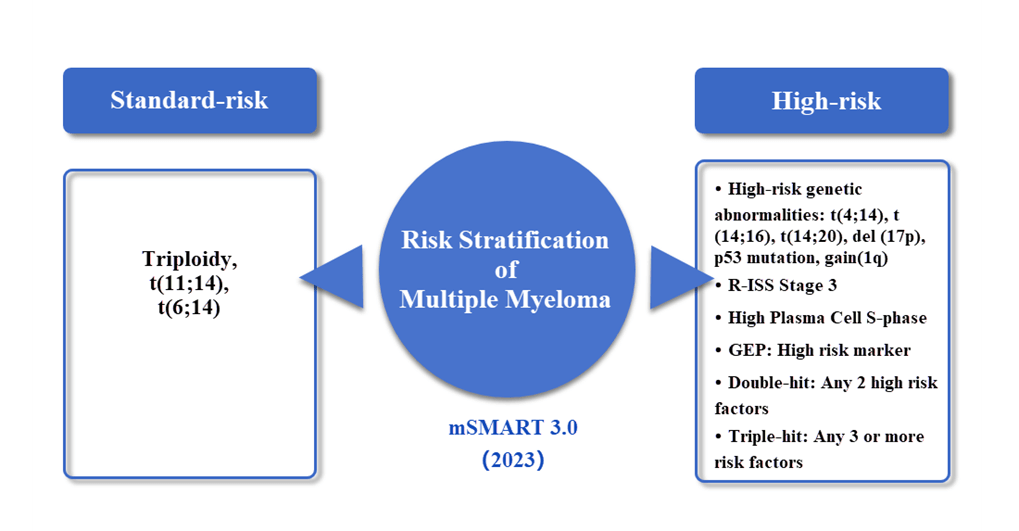
Risk stratification of multiple myeloma helps doctors determine the prognosis and treatment regimens of multiple myeloma. Currently, multiple myeloma is roughly divided into two categories, standard-risk and high-risk. According to the 2023 Mayo Clinic guidelines (mSMART 3.0), the risk stratification of multiple myeloma is as follows6:
The staging of multiple myeloma is also closely related to disease prognosis and choice of treatment regimen. The commonly used clinical staging systems are the International Staging System (ISS) and the Revised International Staging System (R-ISS). The ISS staging system includes beta-2 microglobulin in the staging consideration. The R-ISS staging system has been further revised to include LDH and certain cytogenetic high-risk factors in the staging consideration7.
| Stage | ISS | Median OS (months) | R-ISS | 5-year median OS rate (%) |
|---|---|---|---|---|
| Stage I | Beta-2 microglobulin < 3.5 mg/L and albumin ≥ 35 g/L | 62 | ISS Stage I and non-cytogenetic high-risk patients with normal LDH | 82 |
| Stage II | All patients who do not meet the criteria for Stage I and II | 44 | All patients who do not meet the criteria for R-ISS Stage I and II | 62 |
| Stage III | β2-MG ≥ 5.5mg/L | 29 | ISS Stage III with cytogenetic high-risk patients or LDH levels above normal | 40 |
*Cytogenetic high-risk refers to the detection of del(17p), t(4;14), t(14;16) by fluorescent in situ hybridization during interphase
What Can Be Done After Diagnosing Multiple Myeloma?
- Learning about disease-related knowledge
- Management of unhealthy emotions in time
- Compliance with treatment
- Paying attention to new treatment methods (going abroad for referral to receive car-T therapy)
- Closely monitoring of treatment-related adverse reactions
Related Article
References:
1. Liu J, et al. J Hematol Oncol. 2019 Dec 10;12(1):136.
2. NCCN Guidelines for Patients. Multiple Myeloma. 2023.
3. Brian G.M. Durie. International myeloma foundation. Do You Have Myeloma? Last Medical Review: September 11, 2019
4. Chinese Medical Doctor Association, Hematology Branch, et al. Chinese Journal of Hematology. 2020;59(5):341-6.
5. Brian G.M. Durie. International myeloma foundation. What Are MGUS, Smoldering Multiple Myeloma, and Active Myeloma?
6. Ailawadhi S, et al. Mayo Clin Proc 2023. Treatment of Newly Diagnosed Myeloma.
7. Chinese Medical Doctor Association, Hematology Branch, Chinese Society of Hematology, Chinese Medical Association. Chinese Journal of Hmatology, 2022, 61(5):51-58.